A New Solution to Detecting Impaired Workers
An employee’s ability to perform work tasks correctly, efficiently, and above all safely, is extremely important because their inherent value to any company is predicated on these factors. Even the most experienced and skilled worker cannot contribute to improving the company’s bottom line when impaired and becomes a liability to themselves, the company, and their co-workers.
The state of being impaired has become more difficult to identify as complications arising from the COVID-19 pandemic, fatigue, opioid abuse, marijuana legalization, chronic homelife stress, and mental health problems, converge to create workplace environments that are increasingly unstable. The conventional drug tests that have been used for decades simply cannot account for such a diverse combination of potential stressors that cause impairment.
For instance, the increasing number of employees who use marijuana in the workplace is just one example of the predicament facing employers. Marijuana’s active “THC” chemical, its main psychoactive compound, may be detected in a Monday drug test when in fact the employee consumed it the previous Friday night when by Monday its effects had completely dissipated. To further muddy the waters, several factors contribute to the longevity and intensity of impairment, including body weight, frequency of use, and the potency of the marijuana itself, which can vary considerably.
Employers are very concerned about these dysfunctional workers, as one would expect. A 2021 study (updated in June of 2022) by the National Safety Council (NSC) is instructive. In its Executive Summary, the report found that multiple recent reports indicate spikes in opioid overdoses and ongoing concerns about mental distress and substance use disorders related to COVID-19. As a result, employers are finding themselves with an expanding list of issues that are threatening the safety and wellbeing of their employees.
The data for the study was gathered from 350 employer using online surveys. The agency found that:
- Nearly all (90%) said they were concerned about alcohol, illicit opioids, mental health disorders, chronic stress, and illicit prescription opioids in their workplaces
- More than half of respondents (52%) said impairment was decreasing the safety of their workforce
- Most respondents (77%) viewed impairment as an important consideration when determining an employee’s fitness for duty
- Two-thirds (68%) viewed impairment as a justifiable reason to dismiss an employee
What options do employers have to identify and remove impaired and unsafe employees, if any? Fortunately, a new approach to this complex issue has become available. Known as Impairment Detection Technology (IDT), the NSC indicates that it can be used to determine the real-time fitness of workers by identifying multiple forms of impairment.
Despite the availability of this technology, only 16% of respondents to the NSC survey stated that it is being used at their companies but 79% and 70 % indicated that they were either somewhat or very interested in finding out more about its potential use to detect mental health and opioid impairment.
Considering the seriousness of the problem, employers should take time to investigate what the marketplace offers regarding impairment identification. “Detecting when a worker is impaired is critical for the safety, health, and wellbeing of an organization’s workforce,” said Jenny Burke, vice president of impairment practice at NSC in a press release.
For more information regarding Impairment Detection Technology, click on the following link:
https://www.nsc.org/faforms/impairment-detection-technology-report
Health Officials Concerned About Monkeypox Outbreak
Since the outbreak of the COVID-19 pandemic in 2020, the workplace has been forced to become involved with communicable disease prevention and control. Although OSHA has always required employers to provide a “safe and healthful workplace”, preventing the spread of viruses and bacteria was never really considered part of the equation for most businesses until COVID. An occasional outbreak of flu perhaps occurred before 2020 but never did workplaces experience anything like COVID. Employers needed to learn quickly about sanitation, social distancing, mask wearing, and much more.
The “shrinking world” effect is partly, if not completely, to blame for the current situation. Increased world-wide travel and the resulting intermingling of peoples from all over the globe provides a perfect pathway for pathogens to spread. This means that diseases developing thousands of miles away from the United States are more than likely to arrive here eventually.
Naturally, the work environment is not immune to this phenomenon, so just when employers believed that they could lower their guards somewhat as COVID receded into the background, health and medical authorities began sounding the alarm regarding the next potential threat, monkeypox. Although this disease has fewer than 20,000 cases to date in the U.S., and experts claim is far less communicable than COVID, there still is some lingering uncertainty about its future impact on the population.
Believing that an epidemic outbreak is unlikely could be a mistake. Remember the almost casual approach top US leadership took when COVID first appeared in the U.S. followed by confusing and sometimes contradictory guidance being offered by the authorities? This is happening again to some extent because, like COVID, there is yet no consensus among medical and epidemiological professionals about how the contagion spreads.
At this point, employers should at least have a basic understanding of this virus before it becomes a problem (hopefully it never will). Below are some of the currently known facts about the disease:
- Monkeypox resembles smallpox because both are members of the same viral family and was first identified in humans in West Africa in 1970. Smallpox has been infecting humans for thousands of years but was declared eradicated world-wide in 1980 because of effective vaccination programs.
- Monkeypox sufferers may experience fever, headache, muscle ache, backache, chills, and extreme fatigue. Visible indicators of a monkeypox infection are pustules on the body, initially on the hands and feet, which then may spread to the genitals, the inside of the mouth and even the eye (cornea). Duration of the illness is usually 30 days but one in ten cases is fatal.
- The World Health Organization (WHO) recommends a PCR (Polymerase Chain Reaction) test which detects the presence of the virus and is a similar test commonly used to detect COVID. Rashes, WHO states, are typical for many diseases so only a PCR will distinguish monkeypox from other viral diseases such as chicken pox and measles.
- The current general belief in the medical and epidemiological communities, which of course is subject to change as more information becomes available, is that monkeypox is spread from human to human via body fluids, lesions, respiratory droplets or by contacting an infected person’s clothes or bedding.
- Inoculating the population is in its infancy. The original smallpox vaccine is no longer available to the general-public and a newer vaccine was approved for the prevention of smallpox and monkeypox in 2019 but is not yet widely available.
Employers have been “down this road” before so staying abreast of current news regarding this virus is the prudent thing to do. At this point, monkeypox is considered a minor outbreak, but the recent COVID experience teaches that the situation can change rapidly. Informed vigilance is the best policy until the danger has passed or an effective vaccine becomes widely available that will prevent another COVID-like pandemic.
______________________________________________________________________________
Safety Glasses Work Only When Worn
The well-known Hierarchy of Controls inverted pyramid from the National Institute for Occupational Safety and Health (NIOSH) illustrates hazard avoidance strategies, from most desirable to least. Personal protective equipment (PPE) is the last line of defense against injury because, when all other accident prevention measures fail, what a worker wears may mean the difference between being injured or not.
Among the most basic and important pieces of PPE are safety glasses, and for good reason. Eyes are by far the most essential of the five senses because up to 80% of a person’s perceptions of the world are sight dependent. An individual’s movements, tasks they perform, and personal interactions they engage in, are possible only because of information sent by the eyes to the brain. Good vision is crucial because connects people with their surroundings, with each other, keeps them safe, and helps maintain mental acuity.
It is a given that working in many industrial, construction, and warehouse environments can be hazardous to the eyes. Each day, about 2,000 U.S. workers sustain an eye injury that requires medical treatment. Many suffer temporary loss of sight or suffer injuries that eventually heal but others have permanent-partial loss of sight or even lose it completely. The fact is, however, that 90 percent of eye injuries are preventable if workers wear safety glasses which have been relied upon to protect workers’ eyes for over a hundred years.
As with any other type of PPE, their effectiveness depends upon whether workers utilize them or not. Glasses that are stored in a shirt pocket, on a workbench, or in a tool chest cannot prevent eye injuries. Why do so many workers dislike them when their benefits are so obvious? Quite often their usefulness has been limited by the tendency to “fog up” when exposed to various environmental factors such as rapid changes in temperature and humidity levels which can cause a layer of minute water droplets (fog) to form on the lenses. Worker exertion and wearing face masks also contribute to this problem.
Ironically, instead of preventing injuries, they may create a hazard by inhibiting a worker’s ability to see where their hands are in relation to machinery or tools being used. Solving the fogging problem has been a priority for safety glass manufacturers for years but with generally poor results. Assorted pastes, sprays, and other treatments to lenses have been available beginning in the 1960’s when NASA developed anti-fogging treatments for application to astronaut face shields.
Fortunately, modern anti-fog products have improved greatly and far out-perform pastes and sprays of yesteryear by preventing water droplets from forming on lens surfaces. By treating them with a variety of chemical coatings that fall into two categories, either hydrophobic or hydrophilic, the droplets that cause fogging are never able to form.
Safety glasses featuring either chemical will prevent fogging but are most effective when used under the right conditions. Hydrophobic lenses disperse water and are recommended for high or extreme moisture locations or where workers regularly travel back and forth between environments with different ambient temperatures. Hydrophilic lenses absorb water so are most efficient when used in low to moderate moisture work areas.
Regardless of the selection process, the fact remains that all workers must be provided with, and required to wear, safety glasses that are appropriate for their respective activities, because eye injuries are preventable.
************************************************************************************
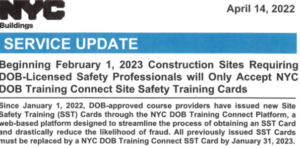
For our clients who preform work within the five boroughs of NYC Please take note of the service update regarding the new SST cards requirement issued back in April of 2022. Questions can be submitted on line at www.nyc,gov/dobhelp
Please direct any questions or concerns to:
The Safety Division at Hamond Safety Management
Anthony Vacchio, avacchio@hamondgroup.com 516-762-4224